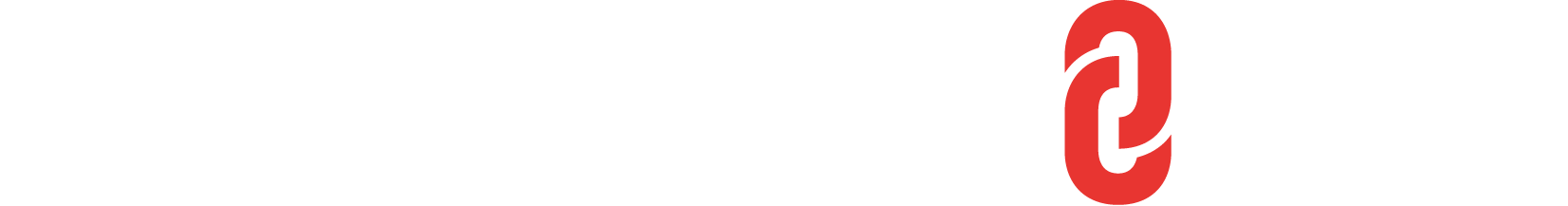
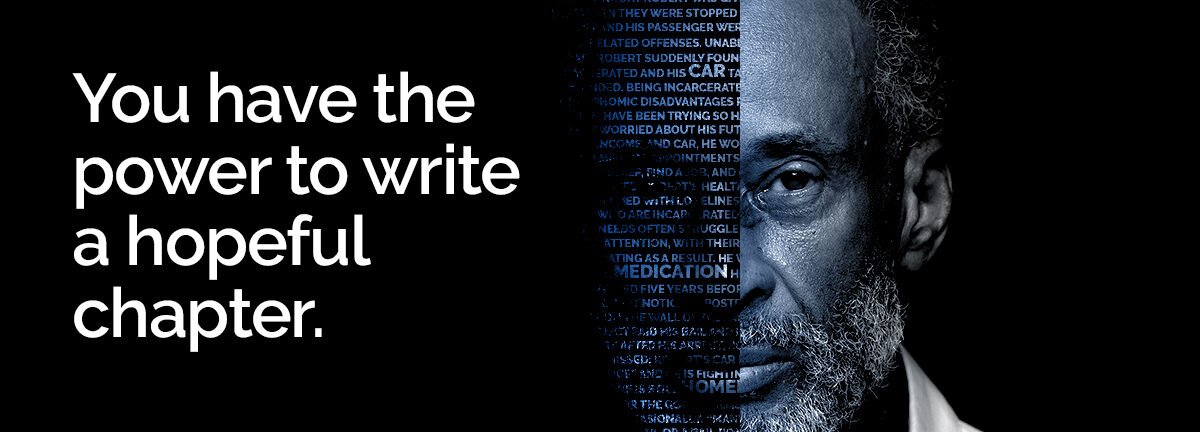
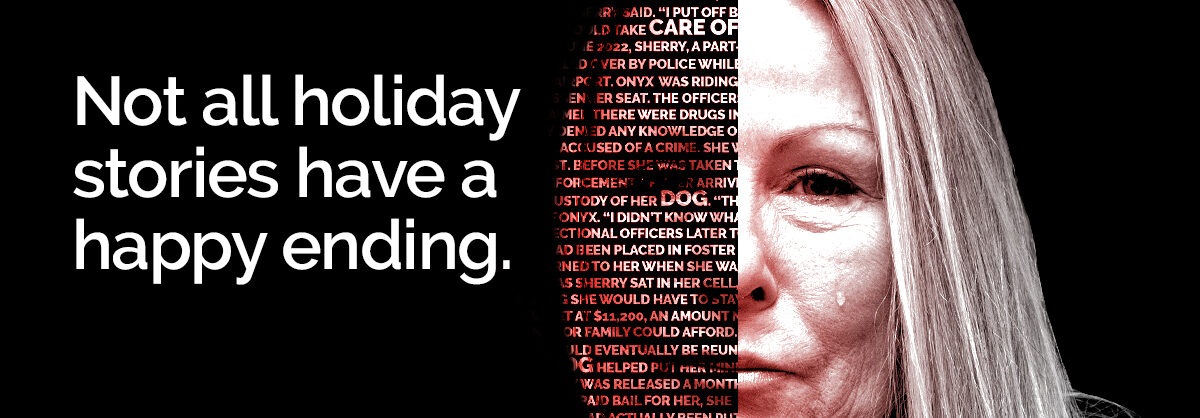
Women are the fastest growing group of incarcerated people and the vast majority are of reproductive age. Reproductive health care – which refers to a gamut of services, including but not limited to contraception and pregnancy care – mirrors the state of health care more broadly in jails: it’s inadequate, and often dangerous. Stories from our clients, including Maribeth and Ashley, highlight the dismal reality of being both pregnant and incarcerated as a result of unaffordable cash bail.
To better understand the state of reproductive care and access in U.S. jails, we spoke with Dr. Carolyn Sufrin, associate professor of gynecology and obstetrics at Johns Hopkins University.
- Sufrin: It depends – and that is part of the story. The availability and quality of reproductive health care in U.S. jails vary widely depending on what county and what jail you’re talking about. There are some jails that provide access to a reasonable measure of reproductive health care by qualified providers; but there are many others that do not.
- Sufrin: It has huge implications for the health and well-being of individuals, families, and communities. The vast majority of women in the United States who are incarcerated are of childbearing age, and most of them are mothers and primary caregivers to children. This is a large number of people we’re talking about. Most women who are incarcerated in jails don’t stay there very long – we must think about jail, health care, and reproductive health care not as isolated issues, but as integral parts of community health.
- Sufrin: One prime example of disruption of care involves access to contraception. Our research has found many jails do not allow people to continue a method of contraception – like birth control pills or the patch – while they are in jail. If you think about it, if someone is in jail for even just a few days, and they’re not allowed to continue their prescribed medication, then when they return to their communities and if they have sex, they could be at risk of an unplanned pregnancy. You can apply this logic of disruption to many other aspects of reproductive health care.
- Sufrin: When we sampled 22 state prison systems and six jails – including the five largest jails – we found that access to abortion is variable. There were two jails that did not allow individuals to access abortion. Even at the jails and prisons that did allow abortion, there was variability: some had policies that only allowed abortion in the first trimester – when that might have been out-of-step with state law – and some required women to fund their own abortions. We did this study before Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade; this was when we had constitutional protections for abortions.
- Sufrin: We must invest in alternatives to incarceration and robust safety net services. We have seen this is possible in Cook County (IL), one of the largest jails in the country. Several years ago, the County decided to release on recognizance pregnant individuals in their third trimester who were charged with certain non-serious charges, so they would not have to endure the variability of care in jail or go into labor in custody. We need more models like this. Until that time comes, though, we absolutely need standardization and oversight of quality reproductive health care, as well as data collection for these issues at all levels of incarceration, including local jails.
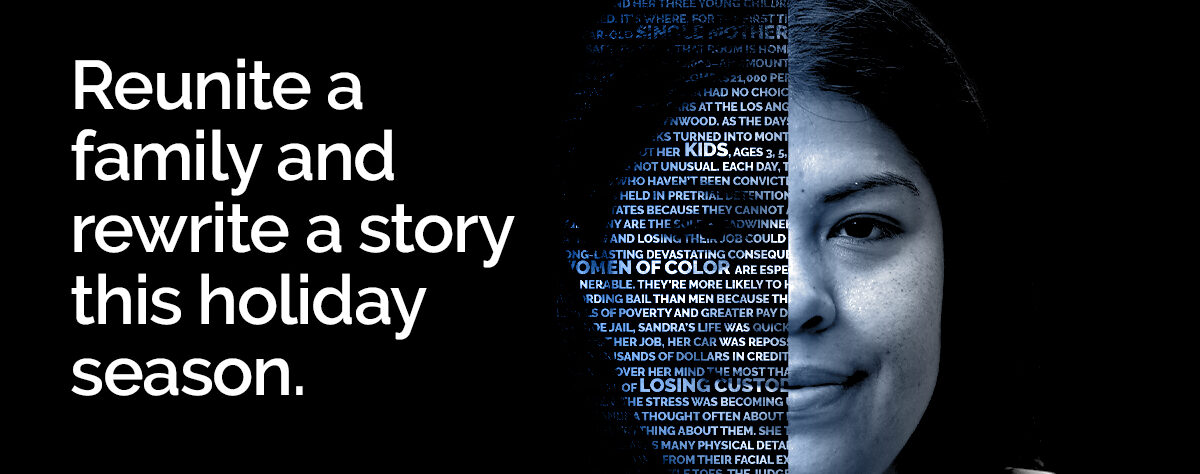
While financial barriers to paying bail can lead to people being unjustly confined in jails with subpar healthcare, particularly in reproductive services, there is a glimmer of hope. At The Bail Project, we’ve already assisted nearly 30,000 low-income individuals in evading the detrimental health impacts of incarceration by securing their release. Our efforts are a testament to the ongoing struggle for a justice system where access to freedom and adequate healthcare isn’t dictated by financial standing, but is a fundamental right for all.
Our conversation has been edited for length and clarity.
Thank you for reading. The Bail Project is a 501(c)(3) nonprofit organization that is only able to provide direct services and sustain systems change work through donations from people like you. If you found value in this article, please consider supporting our work today.